Just launched
How can we unlock AI’s full potential in healthcare?
Learn new insights from patients and healthcare professionals in the 2025 Future Health Index report
A better vision for mobile ultrasound
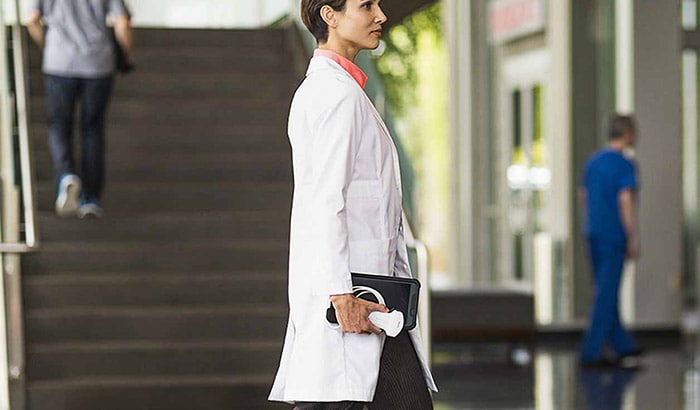
The Lumify app enhances imaging to help confidently and quickly assess internal medicine patients.
